2A 40-year-old man with adult polycystic kidney disease is brought to the emergency room in a coma. CT scan of the head demonstrates a subarachnoid hemorrhage without parenchymal hemorrhage. Which of the following is the most likely source of the bleeding? A. AV malformation B. Bridging veins C. Charcot-Bouchard aneurysm D. Circle of Willis E. Middle meningeal artery Answer
3An unconscious patient with sepsis in the intensive care unit undergoes a 2-hour period of severe hypotension. Blood chemistries taken during the following 48 hours show rising creatine kinase MB fraction (CK-MB), peaking at 5 times the upper limit of normal. ECG findings are equivocal, with some degree of flat S-T segment depression over several leads. Which of the following is the most likely diagnosis? A. Prinzmetal angina B. Stable angina C. Subendocardial infarction D. Transmural infarction E. Unstable angina Answer
4A 65 year-old man is admitted to the coronary care unit with a diagnosis of a large myocardial infarct (MI) of the left ventricle. On his 6th postinfarct day, he goes into shock and dies, manifesting signs and symptoms of cardiac tamponade. Which of the following complications is the most likely cause of this patient's death? A. Aortic dissection B. Extension of previous MI C. Fatal arrhythmia D. Rupture of the left ventricular wall E. Rupture of papillary muscle Answer
5A newborn appears normal at birth, but develops vomiting and diarrhea accompanied by jaundice and hepatomegaly within the first few weeks of life. Within months, the baby has obvious cataracts and ascites. The infant is switched to a milk-free diet, which stabilizes but does not completely reverse his condition. By one year of age, he has developed mental retardation. Which of the following is the most likely diagnosis? A. Cystic fibrosis B. Galactosemia C. McArdle's disease D. Von Gierke's disease E. Wilson's disease Answer
6A 25-year-old man presents with headache, dizziness, and claudication. Blood pressure measurements reveal hypertension in the upper limbs and hypotension in the lower limbs. Which of the following additional findings would be most likely in this case? A. Aortic valvular stenosis B. Notching of inferior margins of ribs C. Patent ductus arteriosus D. Pulmonary valvular stenosis E. Vasculitis involving the aortic arch Answer
7A patient has a tiny (0.2 cm), but exquisitely painful tumor under the nail of her index finger. Prior to surgery to remove it, local anesthetic block to a branch of which of the following nerves would be most likely to achieve adequate anesthesia? A. Axillary nerve B. Median nerve C. Musculocutaneous nerve D. Radial nerve E. Ulnar nerve Answer
8Tissue from a spontaneous abortion is submitted to the laboratory, where an astute pathologist notes the presence of mature fetal tissue that contains Barr bodies. The fetus may have had which of the following genotypes? A. Classic Turner syndrome (45, X) B. Edward's syndrome (47, XY+18) C. Klinefelter's syndrome (47, XXY) D. Normal male (46, XY) E. XYY syndrome (47, XYY) Answer
9A 78-year-old woman is brought to the emergency department because of slowly developing confusion over the past ten days. Careful physical examination demonstrates a relatively small laceration of the scalp. CT of the head would be most likely to reveal which of the following? A. Epidural hematoma B. Mixed parenchymal and subarachnoid hemorrhage C. Multiple tiny hemorrhages of the putamen D. Subarachnoid hemorrhage E. Subdural hematoma Answer
10A 22-year-old woman presents to her physician with amenorrhea, weight loss, anxiety, tremor, heat intolerance and palpitations. Laboratory examination is consistent with hyperthyroidism, and the physician prescribes propylthiouracil. The patient's response to propylthiouracil is disappointing, and the symptoms recur, then worsen. Subtotal thyroidectomy is successfully performed, but following the surgery, the woman is extremely hoarse, and can barely speak above a whisper. This hoarseness is most probably related to damage to a branch which of the following cranial nerves? A. Facial B. Glossopharyngeal C. Hypoglossal D. Trigeminal E. Vagus Answer
11A 24-year-old female is brought to the emergency room after threatening to kill herself by cutting her wrists. She has multiple scars on her wrists, which she admits were caused by prior suicide attempts. She states she is very angry at her boyfriend, who left her for another woman. She previously thought her boyfriend was an angel and now she thinks he is a monster. She feels very empty inside. While smiling, she states that she is depressed. During the interview, she drops to the ground, but continues to talk while lying on the floor . She believes nobody understands her. What is her underlying personality disorder? A. Antisocial B. Borderline C. Histrionic D. Narcissistic E. Schizoid Answer
12A high school basketball player passes out in the middle of a game. He is rushed to the emergency room, where he regains consciousness. He claims that just before he fainted, he had difficulty breathing and experienced palpitations. On physical exam, he has a bifid apical impulse and a coarse systolic murmur at the left sternal border. The echocardiogram reveals ventricular hypertrophy with asymmetric septal thickening. Which of the following would increase the intensity of his heart murmur? A. Elevating his legs B. Increasing sympathetic tone C. Performing the Valsalva maneuver D. Squatting Answer
13A 63-year-old man complains of trouble swallowing and hoarseness. On physical exam, he is noted to have ptosis and a constricted pupil on the left, and a diminished gag reflex. Neurological examination shows decreased pain and temperature sensation on the left side of his face and on the right side of his body. Which of the following vessels is most likely occluded? A. Anterior inferior cerebellar artery (AICA) B. Anterior spinal artery C. Middle cerebral artery (MCA) D. Posterior cerebral artery (PCA) E. Posterior inferior cerebellar artery (PICA) Answer
14Examination, at autopsy, of the brain of a man who died in an intensive care unit demonstrates bilateral, linear, parasagittal areas of coagulative necrosis in the junctional zone between the anterior and medial cerebral arterial systems. Which of the following is the most likely etiology? A. Bacterial infection B. Fungal infection C. Ischemia D. Tumor E. Viral infection Answer
15A 55-year-old woman presents to her physician after several episodes of syncope. Physical examination is remarkable for a low-pitched "plopping" sound during mid-systole. Two-dimensional echocardiography demonstrates a ball-valve type obstruction of the mitral valve. Which of the following would most likely be observed if the cause of the obstruction were biopsied? A. Benign glandular tissue B. Densely packed smooth muscle C. Densely packed striated muscle D. Malignant glandular tissue E. Scattered mesenchymal cells in a myxoid background Answer
16The presence of which of the following features in an atherosclerotic plaque indicates that it has become a complicated lesion? A. Cholesterol crystals B. Chronic inflammatory cells C. Intimal smooth muscle D. Lines of Zahn E. Necrotic cell debris Answer
17A 46-year-old woman presents to her physician with "double vision" and is unable to adduct her right eye on attempted left lateral gaze. Convergence is intact. Both direct and consensual light reflexes are normal. Which of the following structures is most likely to be affected? A. Left oculomotor nerve B. Medial longitudinal fasciculus C. Right abducens nerve D. Right oculomotor nerve E. Right trochlear nerve Answer
18A patient arrives in the emergency room after having suffered severe head trauma in a motorcycle accident. Radiographic studies of the head reveal a basilar skull fracture in the region of the foramen ovale. Which of the following functional losses would most likely be related to this injury? A. Loss of abduction of the eye B. Loss of sensation over the forehead C. Loss of sensation over the zygoma D. Loss of taste sensation on the anterior 2/3 of the tongue E. Paralysis of muscles of mastication Answer
19A 64-year-old man has a myocardial infarction, and is hospitalized. He is seen by a cardiologist, who orders echocardiographic studies, which demonstrate a portion of the apex of the left ventricle that bulges outward during systole and inward during diastole. This finding is most likely related to disease involving which of the following structures? A. Aortic valve B. Circumflex artery C. Left anterior descending artery D. Mitral valve E. Tricuspid valve Answer
20A mailman gets a severe bite wound from a pit bull guarding a junkyard. The wound is cleansed and he receives a booster injection of tetanus toxoid and an injection of penicillin G. Several days later, the wound is inflamed and purulent. The exudate is cultured on blood agar and yields gram-negative rods. Antibiotic sensitivity tests are pending. The most likely agent to be isolated is A. Bartonella henselae B. Brucella canis C. Clostridium tetani D. Pasteurella multocida E. Toxocara canis Answer
21A 7-year-old boy is referred to a specialty clinic because of digestive problems. He often experiences severe abdominal cramps after eating a high fat meal. He is worked up and diagnosed with a genetic defect resulting in a deficiency of lipoprotein lipase. Which of the following substances would most likely be elevated in this patient's plasma following a fatty meal? A. Albumin-bound free fatty acids B. Chylomicrons C. HDL D. LDL E. Unesterified fatty acids Answer
22A 10-year-old girl who is a suspected victim of child abuse is referred to a psychologist for evaluation. As part of her workup, the patient is asked to construct a story based on pictures. Which of the following psychometric measures was utilized? A. Minnesota Multiphasic Personality Inventory B. Myers-Briggs Personality Inventory C. Rorschach Test D. Thematic Apperception Test E. Type A and B Behavior Patterns Test Answer
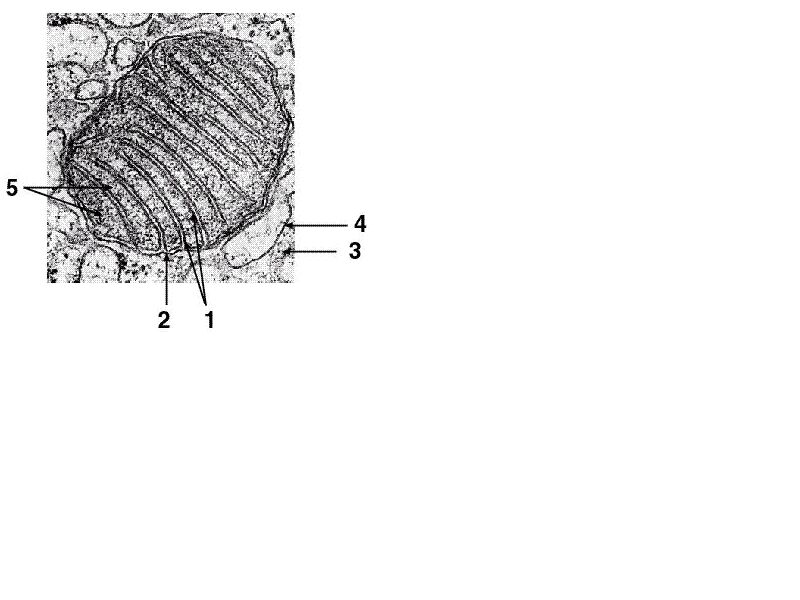
23Which of the following enzymes is located at arrow 1 in the electron micrograph above? A. Carnitine acyltransferase II B. Fatty acyl CoA synthetase C. Glucose-6-phosphate dehydrogenase D. Hexokinase E. Pyruvate kinase Answer
24A 22-year-old female college student is brought into the emergency room by the police, who found her walking back and forth across a busy street, talking to herself. The young woman appears to be oriented with respect to person, place, and time. Her first hospital admission was two months ago for a similar condition. During a psychiatric interview, she has difficulty concentrating, and seems to hear voices . A phone call to her sister provides the additional information that the girl dropped out of school three months ago and has been living on the street. Urine toxicology is negative. This patient is most likely exhibiting the signs and symptoms of A. schizoaffective disorder B. schizoid personality disorder C. schizophrenia D. schizophreniform disorder E. schizotypal personality disorder Answer
25A 42-year-old man has just been informed that he has poorly differentiated small cell carcinoma of the lung. When asked if he understands the serious nature of his illness, the patient proceeds to tell his physician how excited he is about renovating his home. This patient is exhibiting A. denial B. displacement C. projection D. rationalization E. reaction formation F. sublimation Answer
26An increase in which of the following best explains the mechanism by which the cardiac output increases in severe anemia? A. Arteriolar diameter B. Blood viscosity C. Peripheral vascular resistance D. Splanchnic blood flow E. Tissue oxygen tension Answer
27A 2-year-old retarded child is evaluated by a metabolic specialist. The child's history is significant for failure to thrive and progressive neurologic deterioration, including deafness and blindness. Physical examination is remarkable for hepatosplenomegaly, as well as a cherry-red spot on funduscopic examination. These symptoms are consistent with a diagnosis of A. Hunter syndrome B. Niemann-Pick disease C. Pompe's disease D. tyrosinosis E. von Gierke's disease Answer
28An 8-month-old female child is brought to medical attention because her first four teeth show several discrete, discolored, circumferential bands that show very little enamel. Excessive levels of which of the following may have produced this defect? A. Bilirubin B. Fluoride C. Parathormone D. Thyroid hormone E. Vitamin C Answer
29Which of the following complications is currently the major limitation to the long-term success of cardiac transplantation? A. Allograft rejection B. Graft arteriosclerosis C. Graft atherosclerosis D. Opportunistic infections E. Lymphoma Answer
30A child develops a tumor of the cerebellum. Biopsy reveals evidence of both neuronal and glial differentiation. Which of the following is the most likely diagnosis? A. Astrocytoma B. Glioblastoma multiforme C. Medulloblastoma D. Meningioma E. Oligodendroglioma Answer
31A 56-year-old man visits his physician with complaints of complete exhaustion after mowing the lawn in his small front yard. He also complains of dizziness, irritability, difficulty sleeping, and loss of libido. On physical examination, the man's skin, conjunctiva, and oral mucosa are pale. A blood test indicates the man's hemoglobin is 7 g/dL. Which of the following findings is also likely to be present in this man? A. Bradycardia B. Cyanosis C. Low stroke volume D. Warm hands E. Wide pulse pressure Answer
32A 55-year-old man had been in good health since receiving a heart transplant for severe atherosclerotic disease. Five years after transplantation, the patient died suddenly, without any premonitory symptoms, while working in his garden. He had been maintained on cyclosporin since his transplant. Which of the following complications would most likely be found at autopsy in the transplanted heart? A. Allograft rejection B. Atherosclerosis of coronary arteries C. Graft vascular disease D. Hyaline arteriolosclerosis E. Hyperplastic arteriolosclerosis Answer
33An elderly lady is brought to the emergency room after drinking insecticide that she thought was tea. After her stomach is pumped , her sense of smell is tested and it is found that she can not distinguish common smells (e.g., an orange, coffee). CT scan of the head demonstrates a mass in the olfactory groove area. The axons likely compressed by this mass project to which of the following structures? A. Insula B. Nucleus ambiguus C. Post-central gyrus D. Pre-central gyrus E. Pyriform cortex Answer
34A 27-year-old man develops bilateral parotid gland swelling and orchitis, and is generally ill with fever of 102° F. Which of the following substances is most likely to be significantly elevated in the patient's serum? A. Alanine aminotransferase (ALT) B. Amylase C. Aspartate aminotransferase (AST) D. Ceruloplasmin E. Creatine phosphokinase, MB isoenzyme (CPK-MB) Answer
35A 55-year-old man presents to the emergency room with crushing substernal pain and left shoulder pain of 2 hours duration. The pain is not relieved by sublingual nitroglycerin, and the electrocardiogram shows ST elevation in several leads. Aspirin and streptokinase therapy are initiated, and the patient is admitted to the intensive care unit. The next morning, serum cardiac enzymes are elevated to 4 times the upper limit of normal, and the electrocardiographic changes are still present. Which of the following is the most likely diagnosis? A. Prinzmetal's angina B. Stable angina C. Subendocardial infarction D. Transmural infarction E. Unstable angina Answer
36Which of the following amino acids is post-translationally hydroxylated in the cytoplasm of fibroblasts? A. Cysteine B. Glycine C. Proline D. Serine E. Tyrosine Answer
37Microscopic examination of a cancer cell reveals a cell in an abnormal telophase in which three clusters of chromosomes are seen. An abnormality of which of the following would be most likely to produce this alteration? A. Chiasma B. Mitotic spindle C. Mosaicism D. Polar body E. Synapsis Answer
38A 58-year-old man with fainting spells and exercise intolerance is found to have a bicuspid aortic valve with marked aortic stenosis. Which of the following physical findings would be prominent in this patient? A. Diastolic murmur B. Heave at left parasternal border C. Loud S2 heart sound D. Loud S3 heart sound E. Weak peripheral pulse Answer
39A 57-year-old female is found unconscious on her kitchen floor after having suffered a myocardial infarction. She has pulmonary edema and distended jugular and peripheral veins. A midsystolic gallop is heard upon chest auscultation. EKG shows prominent Q waves in leads II, III, and aVF. Which of the following is most consistent with the patient's condition? Preload Cardiac output PAWP CVP Vascular resistance Mixed venous oxygen A. Increased Decreased Decreased Increased Increased Decreased B. Increased Increased Decreased Decreased Decreased Increased C. Increased Decreased Increased Increased Increased Decreased D. Increased Increased Increased Increased Decreased Decreased E. Decreased Decreased Increased Decreased Increased Decreased F. Decreased Increased Decreased Increased Decreased Increased G. Decreased Decreased Increased Decreased Decreased Decreased Answer
40A 48-year-old man complaining of chest pain is brought to the emergency room. Physical examination followed by echocardiography demonstrates aortic stenosis. His coronary blood flow is increased. Which of the following is the most likely explanation for the increased coronary blood flow in this individual? A. Decreased left ventricular oxygen consumption B. Decreased left ventricular pressure C. Decreased left ventricular work D. Increased cardiac tissue adenosine concentration E. Increased cardiac tissue oxygen concentration Answer
41A 45-year-old man presents to the emergency department with severe headache and vomiting. A CT scan shows a well-circumscribed cystic lesion within the 3rd ventricle; there is no calcium deposition. The cyst is surgically removed. On histologic examination, the wall of the cyst consists of a single layer of mucin-producing columnar epithelium with a ciliated apical surface. Which of the following is the most likely diagnosis? A. Colloid cyst B. Craniopharyngioma C. Cysticercosis D. Echinococcus cyst E. Pilocytic astrocytoma Answer
42A 36-year-old female is brought to the emergency room by her husband who says that she "complained of a severe headache then lost consciousness." She has a history of hypertension and had been on several different medications. The examining physician notes that she is unable to move her arms and legs, but can blink her eyes. When the physician asks her to blink twice if she can hear him, she promptly does so. In which of the following structures is this woman's lesion most likely located? A. Cervical spinal cord B. Medulla oblongata C. Midbrain D. Pons E. Thalamus Answer
43A 71-year-old man has been in excellent health, and practicing competently as an attorney. He is brought to the emergency room following a motor vehicle accident. A workup, including imaging of the spine, thorax, and head, is negative, but the patient is admitted for overnight observation. His injuries include several lacerations to the face and extremities as well as several contusions to the thorax. Three weeks later, he is admitted to the hospital for confusion. A neurologic exam is normal except that he is not oriented to time or place, and can recall only 1 out of 6 objects after 3 minutes. Which of the following is the most likely diagnosis? A. Alzheimer's disease B. Brain metastases C. Epidural hematoma D. Normal pressure hydrocephalus E. Subdural hematoma Answer
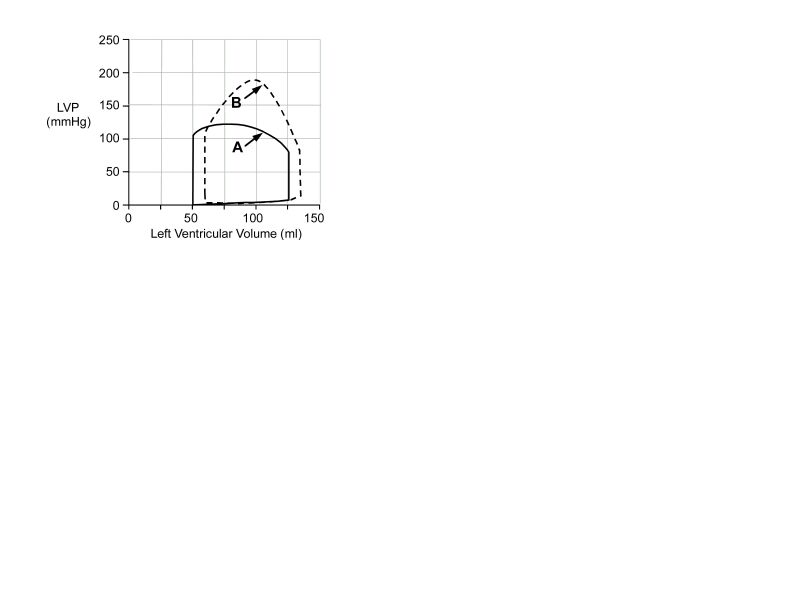
44A work diagram showing changes in left ventricular volume and pressure during one cardiac cycle is shown above for a normal heart (diagram A) and following aortic valvular disease (diagram B). Diagram B shows which of the following compared to diagram A? A. Decreased work for a greater stroke volume B. Decreased work for a lower stroke volume C. Decreased work for the same stroke volume D. Increased work for a greater stroke volume E. Increased work for a lower stroke volume F. Increased work for the same stroke volume Answer
45An 80-year-old woman dies after a long history of progressive memory loss, apraxia, and recurrent episodes of confusion. In the last months of life she was bedridden and unable to recognize familiar faces and objects. The pathologist identifies numerous flame-shaped intracytoplasmic inclusions in neurons of the neocortex and hippocampus. These consist of paired helical filaments (PHFs) on electron microscopy. Which of the following biochemical changes most likely accounts for the development of PHFs in this condition? A. Abnormal degradation of amyloid precursor protein (APP) B. Abnormal phosphorylation of tau C. Accumulation of advanced glycosylation end (AGE) products D. Increased expression of APP E. Precipitation of insoluble a-tubulin Answer
46The activity of which of the following enzymes is directly affected by citrate? A. Fructose-2,6-bisphosphatase B. Isocitrate dehydrogenase C. Phosphofructokinase I D. Pyruvate carboxylase E. 6-phosphogluconate dehydrogenase Answer
47While a physician is using a water-filled syringe to expel wax from the ear canal of an elderly patient, the man suddenly faints. This event can be explained by the fact that the posterior half of the external ear canal receives sensory innervation from the A. auricular branch of the vagus nerve B. auriculotemporal nerve C. greater auricular nerve D. lesser occipital nerve E. vestibulocochlear nerve Answer
48Which of the following structures is found only in Gram-negative microorganisms? A. Cell envelope B. Exotoxin C. Peptidoglycan D. Periplasmic space E. Teichoic acids Answer
49A scientist wishes to study free radical production under ischemic conditions. He decides to produce cerebral ischemia by tying off an artery of the brain. Ligation of which of the following arteries would be most likely to produce significant ischemic damage? A. Anterior cerebral artery at its origin from the internal carotid artery B. Anterior communicating artery C. Middle cerebral artery at its origin from the internal carotid artery D. Posterior cerebral artery at its origin from the basilar artery E. Posterior communicating artery Answer
50A 52-year-old woman has long-standing rheumatoid arthritis (RA) and is being treated with corticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs). Which of the following cardiac complications may arise in this clinical setting? A. Constrictive pericarditis B. Dilated cardiomyopathy C. Hypersensitivity myocarditis D. Hypertrophic cardiomyopathy E. Restrictive cardiomyopathy Answer
Answers
1The correct answer is E. The upper 2/3 of the esophagus contains striated muscle. It is derived from the pharyngeal arches and innervated by the vagus nerve (CN X). The lower 1/3 contains smooth muscle from splanchnic mesoderm and is innervated by the splanchnic plexus. The hypoglossal nerve (choices A and B), or CN XII, moves the tongue. The phrenic nerve (choices A and D), derived from C3, C4, and C5, innervates the muscle of the diaphragm. The glossopharyngeal nerve (choice C), or CN IX, functions in taste, swallowing, and salivation, as well as monitoring the activity of the carotid body.
2The correct answer is D. Two relationships are useful in solving this problem. The first relationship is that adult polycystic kidney disease has a specific association with berry aneurysms involving the circle of Willis and its branches. The second relationship is that spontaneous subarachnoid hemorrhages are most often the result of bleeding from berry aneurysms. The berry aneurysms develop at sites of congenital weakness (near branch points) of the relatively unsupported vessels of the circle of Willis. AV malformations (choice A) tend to produce mixed parenchymal and subarachnoid hemorrhages. Rupture of bridging veins (choice B) produces a subdural hematoma. Rupture of Charcot-Bouchard aneurysms (choice C) can be seen with hypertension (which may complicate adult polycystic kidney disease). Such rupture produces intraparenchymal hemorrhage, which if severe, may spread to the subarachnoid space. Rupture of the middle meningeal artery (choice E) produces epidural hematoma
3The correct answer is C. The high serum CK-MB indicates that the patient has sustained an infarction rather than angina. Subendocardial, rather than transmural, infarction is most likely in the setting of known, prolonged severe hypotension, and the equivocal nature of the ECG findings confirms this diagnosis. Subendocardial infarction occurs in settings of generalized poor perfusion complicated by increased demand or transient vasospasm. Subendocardial muscle tissue is especially vulnerable because it is farthest from the arterial supply. In Prinzmetal angina (choice A) and stable angina (choice B), the CK-MB would not be expected to increase significantly. Transmural infarction (choice D) is not specifically expected in the setting of shock. It produces characteristic ECG changes that are usually localized (unless a very large infarct has occurred) to a few leads. In unstable angina (choice E), an increase in cardiac enzymes may be seen, but is usually less than 2 times the upper limit of normal.
4The correct answer is D. Rupture of the free left ventricular wall is a frequently fatal complication that may occur in the first week after myocardial infarction (MI). At this stage, the infarcted area is composed of friable necrotic myocardium and early granulation tissue. It is during this crucial phase, therefore, that rupture usually occurs. Blood rushes out, filling the pericardial sac and causing compression of the left ventricle. Cardiac tamponade ensues, and the patient usually dies of acute cardiogenic shock. Aortic dissection (choice A) is not a complication of MI, although cardiac tamponade may also follow this acute condition when dissection works its way back toward the aortic root. Aortic dissection usually develops in aortas affected by cystic medial degeneration (CMD), which is due to fragmentation of elastic laminae with accumulation of myxoid material in the aortic media. CMD may be either sporadic or associated with Marfan syndrome. Extension of a previous MI (choice B) may occur in the first few hours or days after MI. It may aggravate or precipitate cardiogenic shock and/or arrhythmias, but it does not cause cardiac tamponade. Arrhythmias (choice C) are frequent complications of MI and are often fatal, producing cardiac arrest (ventricular fibrillation) or aggravating cardiac dysfunction. If infarction involves papillary muscles, these may rupture (choice E). This complication is followed by valvular dysfunction and may manifest with signs of mitral regurgitation and acute congestive heart failure.
5The correct answer is B. Galactosemia is an autosomal recessive disease caused by a deficiency of galactose-1-phosphate uridyltransferase, which is necessary for the metabolism of the galactose derived from milk lactose. The condition should be suspected in infants with growth failure, cataracts, liver disease, aminoaciduria, and mental retardation. A reducing sugar (galactose) is usually present in the urine. Most of the pathology is related to the toxic effects of galactose-1-phosphate. Treatment involves strict dietary lactose restriction, which consists of more than simply withdrawal of milk products, because lactose is also present in many non-diary foods. Strict adherence to the diet can strikingly alter the course of this disease. Cystic fibrosis (choice A) is associated with maldigestion, pancreatic disease, and pulmonary disease. McArdle's disease (choice C) is a glycogen storage disease that selectively affects muscle. Von Gierke's disease (choice D) is a glycogen storage disease affecting the liver and kidneys. Wilson's disease (choice E) is a caused by a metabolic abnormality in the handling of copper that can cause cirrhosis and brain damage, and usually presents in adolescence.
6The correct answer is B. The adult form of aortic coarctation is caused by stenosis in the aortic arch just distal to the left subclavian artery. This leads to hypertension proximal to, and hypotension distal to, the stenotic segment. Hypertension in the upper part of the body manifests with headache, dizziness, and other neurologic symptoms. Hypotension in the lower part of the body results in signs and symptoms of ischemia, most often claudication, i.e., recurrent pain due to ischemia of leg muscles. In addition, collateral arteries between the precoarctation and postcoarctation aorta (eg, the intercostal and internal mammary arteries) enlarge and establish communication between aortic segments proximal and distal to stenosis. Enlarged intercostal arteries produce notching of the inferior margins of the ribs, which can be detected on x-ray and is diagnostic of this condition. Remember that the infantile form of aortic coarctation is associated with patent ductus arteriosus, whereas the adult form is not. Aortic valvular stenosis (choice A) at this age would most likely be caused by a congenitally malformed valve, usually a valve with two cusps or a single cusp. Aortic stenosis manifests with systolic hypotension, recurrent syncope, and hypertrophy/dilatation of the left ventricle. Low systolic pressure is present in the entire body. The isolated form of patent ductus arteriosus (choice C) leads to shunting of blood from the aorta (high-pressure vessel) to the pulmonary artery (low-pressure vessel). Eventually, chronic cor pulmonale develops with resultant right-sided heart failure. Pulmonary valvular stenosis (choice D) is a rare form of congenital heart disease that leads to chronic cor pulmonale and heart failure. Vasculitis involving the aortic arch (choice E) is found in Takayasu arteritis, in which chronic inflammatory changes develop in the aortic arch and its branches (brachiocephalic trunk, left common carotid, and left subclavian arteries). This condition causes stenosis of these arteries; therefore, there will be signs and symptoms of ischemia to the upper part of the body. Since the radial pulses are very weak or absent, this disorder is also known as pulseless disease.
7The correct answer is B. The tumor in question is probably a glomus tumor, which is a benign tumor notorious for producing pain far out of proportion to its small size. The question is a little tricky (but important clinically for obvious reasons) because it turns out that the most distal aspect of the dorsal skin of the fingers, including the nail beds, is innervated by the palmar digital nerves rather than the dorsal digital nerves. Specifically, the median nerve through its palmar digital nerves supplies the nail beds of the thumb, index finger, middle finger, and half of the ring finger. The axillary nerve (choice A), musculocutaneous nerve (choice C), and radial nerves (choice D) do not supply the nail beds. The radial nerve does supply the more proximal skin of the back of the index finger. The ulnar nerve (choice E) supplies the nail beds of the small and half of the ring finger.
8.The correct answer is C. The Barr body, or X chromatin body, is an inactivated X chromosome seen as a small, perinuclear, dark-staining dot in somatic cells with two or more X chromosomes. Barr bodies are seen in any individual born with at least two X chromosomes, including normal females. (47, XXY), the classic karyotype of Klinefelter's syndrome, is defined as male hypogonadism due to the presence of a Y chromosome and two or more X's. As in normal females, one of the X chromosomes becomes a Barr body in Klinefelter's syndrome. Classic Turner syndrome females (choice A) and genotypically normal males (choice D) have only one X chromosome. Thus, no X chromosome is inactivated, and somatic cells do not show any Barr bodies. (47, XY+18) is the karyotype of an Edward's syndrome (choice B) fetus. Although this trisomic phenotype is associated with a characteristic syndrome of physical abnormalities, there is no programmed inactivation of the extra chromosome 18. Thus, no Barr body is produced. XYY syndrome (choice E) is not associated with inactivation of any X chromosomes, so Barr bodies are not present. Like a trisomy involving any of the non-sex-linked chromosomes, the duplicated chromosome is expressed in its entirety.
9The correct answer is E. This history is fairly typical for subdural hematoma. Usually, the patient is elderly or alcoholic and has some degree of brain atrophy, causing the brain to pull slightly away from the skull. This stretches the bridging (penetrating) veins that cross the skull to connect to the cranial venous sinuses, leaving them very vulnerable to rupture after minor head trauma. This type of hematoma is due to venous, rather than arterial, hemorrhage and thus tends to develop rather slowly. Epidural hematoma (choice A) is seen following severe head trauma causing laceration of the middle meningeal artery. Mixed parenchymal and subarachnoid hemorrhage (choice B) can be seen with bleeding from AV malformations. Multiple tiny hemorrhages of the putamen (choice C) are intraparenchymal hemorrhages associated with severe hypertension. Subarachnoid hemorrhage (choice D) can be seen with bleeding from ruptured berry aneurysms.
10The correct answer is E. The recurrent laryngeal nerves are branches of the vagus (CN X), and supply all intrinsic muscles of the larynx except the cricothyroid. The right recurrent laryngeal nerve recurs around the right subclavian artery. The left recurrent laryngeal nerve recurs in the thorax around the arch of the aorta and ligamentum arteriosum. Both nerves ascend to the larynx by passing between the trachea and esophagus, in close proximity to the thyroid gland. The recurrent laryngeal nerves are therefore particularly vulnerable during thyroid surgery, and damage may cause extreme hoarseness. The facial nerve (choice A) innervates the muscles of facial expression, the stapedius muscle, and the lacrimal, submandibular and sublingual glands. It also mediates taste sensation from the anterior two-thirds of the tongue. The glossopharyngeal nerve (choice B) innervates the stylopharyngeus muscle and the parotid gland. Visceral afferents supply the carotid sinus baroreceptors and carotid body chemoreceptors, and mediate taste from the posterior one-third of the tongue. Somatosensory fibers supply pain, temperature, and touch information from the posterior one-third of the tongue, upper pharynx, middle ear, and eustachian tube. The hypoglossal nerve (choice C) innervates the intrinsic muscles of the tongue, the genioglossus, hypoglossus, and styloglossus muscles. The trigeminal nerve (choice D) receives sensory information from the face and also innervates the muscles of mastication.
11The correct answer is B. Characteristics of borderline personality disorder include frantic behavior to avoid abandonment, unstable interpersonal relationships, alternating between idealization and devaluation (splitting), recurrent suicidal gestures or other types of self-mutilatory behavior, feelings of emptiness, and inappropriate intense anger. An antisocial patient (choice A) does not confirm to social norms, is deceitful, impulsive, reckless, irresponsible, and lacks remorse for wrongdoings. One symptom that would suggest histrionic personality disorder (choice C) in this patient is her theatrical exaggeration of her emotions by talking while lying on the floor. A histrionic patient might present with attention-seeking and/or seductive and provocative behavior, but the presence of splitting, recurrent suicidal gestures and anger argue strongly for the diagnosis of borderline personality disorder. A narcissistic patient (choice D) is grandiose and preoccupied with success, feels special and requires admiration, feels entitled, takes advantage of others, lacks empathy, and is arrogant. A schizoid patient (choice E) is usually not interested in relationships or pleasurable activities, is a loner, lacks friends, is emotionally cold, and is indifferent to praise or criticism.
12The correct answer is C. This patient has hypertrophic cardiomyopathy-the most common cause of sudden cardiac death in young patients. It usually causes problems during exertion. Clues to the diagnosis include: dyspnea, palpitations, bifid apical impulse, coarse systolic murmur at the left sternal border, and ventricular hypertrophy with asymmetric septal thickening on echocardiogram. Left ventricular outflow obstruction typically plays an important role in the pathophysiology of this condition. Maneuvers that decrease preload, such as the Valsalva maneuver, will accentuate the heart murmur because they result in less ventricular filling, contributing to greater outflow obstruction. Elevating his legs (choice A), increasing sympathetic tone (choice B), and squatting (choice D) would all increase venous return and would therefore diminish the murmur.
13The correct answer is E. The signs and symptoms in this patient are consistent with occlusion of the posterior inferior cerebellar artery (PICA). PICA is a branch of the vertebral artery (which is itself a branch of the subclavian artery). Occlusion of PICA causes a lateral medullary syndrome characterized by deficits in pain and temperature sensation over the contralateral body (spinothalamic tract dysfunction); ipsilateral dysphagia, hoarseness, and diminished gag reflex (interruption of the vagal and glossopharyngeal pathways); vertigo, diplopia, nystagmus, and vomiting (vestibular dysfunction); ipsilateral Horner's syndrome (disruption of descending sympathetic fibers); and ipsilateral loss of pain and temperature sensation of the face (lesion of the spinal tract and nucleus of the trigeminal nerve). AICA (choice A) is a branch of the basilar artery. Occlusion of this artery produces a lateral inferior pontine syndrome, which is characterized by ipsilateral facial paralysis due to a lesion of the facial nucleus, ipsilateral cochlear nucleus damage leading to sensorineural deafness, vestibular involvement leading to nystagmus, and spinal trigeminal involvement leading to ipsilateral pain and temperature loss of the face. Also, there is ipsilateral dystaxia due to damage to the middle and inferior cerebellar peduncles. The anterior spinal artery (choice B) is a branch of the vertebral artery. Occlusion produces the medial medullary syndrome, characterized by contralateral hemiparesis of the lower extremities and trunk due to corticospinal tract involvement. Medial lemniscus involvement leads to diminished proprioception on the contralateral side, and ipsilateral paralysis of the tongue ensues from damage to the hypoglossal nucleus. The MCA (choice C) is a terminal branch of the internal carotid artery. Occlusion results in contralateral face and arm paralysis and sensory loss. Aphasia is produced if the dominant hemisphere is affected, left-sided neglect ensues if the right parietal lobe is affected, and quadrantanopsia or homonymous hemianopsia occur when there is damage to the optic radiations. The PCA (choice D) arises from the terminal bifurcation of the basilar artery. Occlusion results in a homonymous hemianopsia of the contralateral visual field. Often, there is macular sparing.
14The correct answer is C. The distinctive areas of necrosis described in the question stem are border zone (watershed) infarcts. They occur as the result of severe ischemia, which most profoundly affects the relatively poorly perfused areas at the boundaries between major arterial territories. The areas of necrosis described in the question stem are those most commonly observed, although similar infarcts involving border zones in the brain stem are sometimes also seen. Bacterial infection (choice A) tends to produce either meningitis, cerebritis, or localized infections such abscesses. Fungal infection (choice B) tends to produce either meningitis, vasculitis, granulomas, or abscesses. Tumor (choice D) tends to produce localized masses. Viral infection (choice E) may have a variety of patterns, including meningitis, diffuse encephalitis, or localized necrosis, but would not be expected to produce a distinctive linear pattern.
15The correct answer is E. The most common primary cardiac tumor of adults is atrial myxoma, which typically occurs as a single lesion in the left atrium that may intermittently obstruct the mitral valve. Histologically, these tumors are composed of scattered mesenchymal cells in a prominent myxoid background. Benign glandular tissue (choice A) suggests an adenoma, which is not usually found in the heart. Densely packed smooth muscle (choice B) suggests a leiomyoma, which is not usually found in the heart. Densely packed striated muscle (choice C) suggests rhabdomyoma, which is the most common primary cardiac tumor in children, not adults. Malignant glandular tissue (choice D) suggests carcinoma, which can be metastatic to the heart, but does not usually cause a ball-valve obstruction.
16The correct answer is D. Complicated lesions indicate advanced atherosclerotic disease. They arise in atherosclerotic plaques, and render them more susceptible to sudden occlusion and acute infarction of the supplied tissues. Commonly, the plaque ulcerates or ruptures, and the exposed surfaces, being highly thrombogenic, precipitate thrombus formation. Thrombi are typified by the lines of Zahn, alternating layers of platelets and fibrin (the pale lines) and layers of blood (the dark lines). Beyond thrombus formation, other features of a complicated plaque include hemorrhage into the lesion itself, and microembolism by cholesterol crystals or calcified debris. Furthermore, the weakened media underlying the plaque may develop an aneurysmal dilatation. In general, the clinical significance of atherosclerosis is related to the consequences of complicated lesions. The incorrect options all include features of atheromatous plaques, but do not indicate complicated lesions: Beneath the endothelium of a plaque there is a fibrous cap composed of smooth muscle (choice C), chronic inflammatory cells (choice B) and lipid laden macrophages (foam cells), as well as extracellular material. The core of the lesion, which lies between the intima and the media, is composed of necrotic cellular debris (choice E), with cholesterol crystals (choice A), calcium, and more foam cells.
17The correct answer is B. This patient is suffering from internuclear ophthalmoplegia (INO), which is caused by a lesion of the medial longitudinal fasciculus (MLF). The medial longitudinal fasciculus (MLF) connects the oculomotor (III), trochlear (IV), and abducens (VI) nuclei and is essential for conjugate gaze. A lesion in the MLF will result in the inability to medially rotate the ipsilateral eye on attempted lateral gaze. However, a lesion of the motor fibers of the right oculomotor nerve would also lead to the same symptoms. The way to truly distinguish between an INO from a lesion of the medial rectus muscle or a lesion of the motor fibers of CN III is to determine whether the patient can converge her eyes. If the innervation of the medial rectus muscle is interrupted, the patient will not be able to move the ipsilateral eye medially for either conjugate or dysconjugate (convergence) movements. However, if the lesion is in the MLF, this would only affect conjugate movement, and not convergence, asin this patient. The left oculomotor nerve (choice A) is intact because the light reflexes are normal, and there is no description of any eye movement disorders of the left eye. A lesion of the right abducens nerve (choice C) would result in paralysis of the lateral rectus muscle. This would lead to an inability to abduct the right eye. The right oculomotor nerve (choice D) innervates the medial rectus muscle, which would lead to an inability to adduct the right eye when looking toward the left. (CN III also innervates the superior rectus, inferior rectus, and inferior oblique extraocular muscles.) However, a patient with a lesion of this nerve would also be unable to converge. A patient with a lesion of CN III would also be expected to have the affected eye look "down and out" because of the unopposed actions of the lateral rectus and superior oblique muscles, and ptosis resulting from denervation of the levator palpebrae muscle. Additionally, a lesion of the right oculomotor nerve could affect light reflexes and produce mydriasis if the parasympathetic fibers of this nerve were damaged. The trochlear nerve (choice E) innervates the superior oblique muscle, which depresses, intorts, and abducts the eye. A lesion of this nerve theoretically could produce a slight extorsion of the eye and a weakness of downward gaze. However, a lesion of this nerve often produces only minimal symptoms because of the preserved action of muscles that are innervated by the unaffected oculomotor nerve, and because of a compensatory head tilt.
18The correct answer is E. The mandibular nerve passes through the foramen ovale and may be injured by this fracture. The mandibular nerve is responsible for the innervation of all of the muscles of mastication: the masseter, the temporalis, the medial pterygoid, and the lateral pterygoid muscles. Abduction of the eye (choice A) is produced by the lateral rectus muscle, which is innervated by the abducens nerve. The abducens nerve leaves the cranial cavity and enters the orbit by passing through the superior orbital fissure. Sensation in the skin over the forehead (choice B) is provided by the ophthalmic division of the trigeminal nerve. The ophthalmic division leaves the cranial cavity and enters the orbit by passing through the superior orbital fissure. Sensation in the skin over the zygoma (choice C) is provided by the maxillary division of the trigeminal nerve. The maxillary division leaves the cranial cavity and enters the pterygopalatine fossa by passing through the foramen rotundum. Taste sensation on the anterior 2/3 of the tongue (choice D) is provided by the chordae tympani, a branch of the facial nerve. The facial nerve leaves the cranial cavity and enters the temporal bone by passing into the internal auditory meatus. The chordae tympani leave the temporal bone and enter the infratemporal fossa by passing through the petrotympanic fissure.
19The correct answer is C. The motion described is called "paradoxical movement" and occurs when a portion of the ventricular wall is infarcted and can no longer contract during systole. The site of infarction described is in the distribution of the left anterior descending artery. Valvular disease, including that of the aortic valve (choice A), mitral valve (choice D), or tricuspid valve (choice E) will not cause localized paradoxical movement. The circumflex artery (choice B) supplies the superior part of the posterior wall of the heart, anastomosing there with the right coronary artery.
20The correct answer is D. Pasteurella multocida is a gram-negative rod that is normal flora of the oral cavity of dogs and cats. It often causes a local abscess following introduction under the skin by an animal bite. Most cases occur in children who are injured while playing with a pet. Bartonella henselae (choice A) is a very small, gram-negative bacterium that is closely related to the rickettsia, although it is able to grow on lifeless media. It is the cause of cat-scratch disease (a local, chronic lymphadenitis most commonly seen in children) and bacillary angiomatosis (seen particularly in AIDS patients). In this latter patient population, the organism causes proliferation of blood and lymphatic vessels causing a characteristic "mulberry" lesion in the skin and subcutaneous tissues of the afflicted individual. Brucella canis (choice B) is a gram-negative rod that is a zoonotic agent. Its normal host is the dog, but when it gains access to humans, it causes an undulating febrile disease with malaise, lymphadenopathy and hepatosplenomegaly. The normal route of exposure is via ingestion of the organism. Clostridium tetani (choice C) is a gram-positive spore-forming anaerobic rod. It causes tetanus (a spastic paralysis caused by tetanospasmin, which blocks the release of the inhibitory neurotransmitters glycine and gamma-aminobutyric acid [GABA]). There may be no lesion at the site of inoculation, and exudation would be extremely rare. Toxocara canis (choice E), a common intestinal parasite of dogs, is a metazoan parasite that causes visceral larva migrans. Young children are most likely to be affected, as they are most likely to ingest soil contaminated with eggs of the parasite
21The correct answer is B. After eating a high fat meal, triglycerides are processed by the intestinal mucosal cells. They are assembled in chylomicrons and eventually sent into the circulation for delivery to adipocytes and other cells. Chylomicrons are too large to enter cells, but are degraded while in the circulation by lipoprotein lipase. A defect in this enzyme would result in the accumulation of chylomicrons in the plasma. Albumin-bound free fatty acids (choice A) is incorrect because fatty acids leave the intestine esterified as triglycerides in chylomicrons. HDL (choice C) is not a carrier of dietary fat from the intestine. LDL (choice D) would be not be elevated in this patient after a high fat meal. However, VLDL would be elevated if the patient ate a high carbohydrate meal. In this situation, the carbohydrate would be converted into fat in the liver and sent out into circulation as VLDL. VLDL would be unable to be degraded to LDL and, therefore, would accumulate. A defect in lipoprotein lipase would cause a decrease, not an elevation of unesterified fatty acids (choice E), since the chylomicrons contain esterified fatty acids.
22The correct answer is D. The Thematic Apperception test is a projective test employing pictures depicting ambiguous interpersonal situations that the examinee is asked to interpret. Psychodynamic theory suggests that since the stimuli are vague, the patient projects his or her own thoughts, feelings, and conflicts into his or her responses, providing the examiner insight into the patient's thought and memory content. The Minnesota Multiphasic Personality Inventory (MMPI; choice A), which uses true and false items, is the most popular objective personality test. The Myers-Briggs Personality Inventory (choice B) is based on Jungian theory and assesses basic dimensions of personality (extroversion); it is used extensively in occupational counseling. The patient selects preferred adjectives from groups of choices. The Rorschach Test (choice C) is another projective test that involves asking patients to describe what they see when presented with a series of black and white inkblots. The Type A and B Behavior Patterns Test (choice E) assesses the amount of "driven quality" a person has to their life. Type A's are always "running out of time." This is a verbal test that resembles an interview.
23The correct answer is A. Arrow 1 indicates the inner mitochondrial membrane. Carnitine acyltransferase II is located on the inner face of the inner mitochondrial membrane. It reforms fatty acyl CoA in the mitochondrial matrix (arrow 5) from acyl carnitine, thus preparing it for mitochondrial oxidation. The acyl groups on carnitine are derived from acyl CoA esters synthesized in the outer mitochondrial membrane, which are made from free fatty acids circulating in the blood. Fatty acyl CoA synthetases (choice B) are located in the outer mitochondrial membrane, indicated by arrow 2. Glucose-6-phosphate dehydrogenase, the first enzyme in the pentose phosphate pathway (choice C), hexokinase, the first enzyme in the glycolytic pathway (choice D), and pyruvate kinase (choice E), which produces pyruvate from phosphoenolpyruvate in glycolysis, are all located in the cytosol, indicated by arrow 3. Arrow 4 indicates smooth endoplasmic reticulum.
24The correct answer is D. The patient is suffering from schizophreniform disorder. There has been a marked decline in the level of functioning and she was endangering herself in the middle of the street. Schizophreniform disorder is characterized by schizophrenia-like symptoms, but the duration of symptoms is less than six months (but more than one month). Fully developed psychotic symptoms are typical. In schizoaffective disorder (choice A), alterations in mood are present during a substantial portion of the illness. Although schizoid personality disorder (choice B) produces detachment from social relationships and is characterized by restriction of emotional expression, it is not accompanied by a marked decline in occupational functioning. If the symptoms do not remit after six months or more, then the diagnosis of schizophrenia (choice C) should be made. Schizotypal personality disorder (choice E) is characterized by eccentricities of behavior, odd beliefs or magical thinking, and difficulties with social and interpersonal relationships. Unlike schizophrenia, schizotypal personality disorder is not characterized by a formal thought disorder.
25The correct answer is A. This patient is in denial about his serious illness, and by talking about something totally unrelated, he is trying to avoid the bad news he has just received. Displacement (choice B) involves the transferring of feelings to an inappropriate person, situation, or object (e.g., a man who has been yelled at by his boss takes out his anger on his wife). Projection (choice C) is the attribution of one's own traits to someone else (e.g., a philandering husband accuses his wife of having an affair). Rationalization (choice D) involves creating explanations for an action or thought, usually to avoid self-blame. Reaction formation (choice E) is the unconscious changing of a feeling or idea to its opposite (e.g., a man acts very friendly toward a coworker when in fact he is unconsciously jealous). Sublimation (choice F) involves turning an unacceptable impulse into an acceptable one (e.g., someone with very aggressive impulses becomes a professional boxer).
26The correct answer is A. In severe anemia, diminished transport of oxygen in the blood leads to hypoxia in the tissues. The hypoxia (compare to choice E) causes small arteries and arterioles to dilate, which allows greater-than-normal amounts of blood to return to the heart. In severe anemia, the viscosity of blood (choice B) may decrease by 50% or more because blood viscosity depends largely on the concentration of red blood cells. This decrease in viscosity lowers the resistance to blood flow in the peripheral tissues (i.e., decreases peripheral vascular resistance, choice C) allowing even greater amounts of blood to return to the heart. Blood is often shunted away from the splanchnic vascular bed (choice D) in anemia, which can cause gastrointestinal problems.
27The correct answer is B. Hepatosplenomegaly accompanied by progressive neurologic deterioration should make you think of lipid storage diseases; Niemann-Pick disease is the only lipid storage disease in the answer choices. Niemann-Pick disease is due to a deficiency of sphingomyelinase, leading to an accumulation of sphingomyelin. It is most common among Ashkenazic Jews and generally results in death by age 2. The cherry-red spot is also a characteristic of Tay-Sachs disease, but hepatosplenomegaly suggests Niemann-Pick disease rather than Tay-Sachs. Hunter syndrome (choice A) is a mucopolysaccharidosis, inherited in an X-linked recessive fashion. Pompe's disease (choice C) is a glycogen storage disease characterized by hypotonia and cardiorespiratory failure. Tyrosinosis (choice D) is a rare abnormality of tyrosine metabolism that would not produce the listed symptoms. von Gierke's disease (choice E) is a severe form of glycogen storage disease characterized by hypoglycemia, hepatomegaly, and renomegaly.
28The correct answer is B. Fluoride excess causes direct injury to ameloblasts, leading to inadequate production of tooth enamel. The resultant defect in enamel production causes recessed and discolored rings on the emerging teeth. Other conditions that cause enamel hypoplasia include inadequate levels of calcium, phosphorus, and vitamins A, C, or D, hypothyroidism, and hypoparathyroidism. Jaundice in the newborn period may cause bilirubin (choice A) deposition in the developing teeth, resulting in pigmented, but otherwise normal teeth. Hyperparathyroidism (choice C), with resultant hypercalcemia, will result in osteoporosis, renal stones, and neuromuscular weakness, but no obvious dental changes. Enamel hypoplasia is associated with hypoparathyroidism. Hyperthyroidism (choice D) characteristically produces cardiac and nervous disturbances, weight loss, hypermetabolism, and proptosis, but does not cause enamel hypoplasia. Hypothyroidism, not hyperthyroidism, produces enamel hypoplasia. Excess dietary vitamin C (choice E) is generally excreted in the urine and produces no systemic pathology. Scurvy, due to inadequate vitamin C, may produce enamel hypoplasia.
29The correct answer is B. Currently, graft arteriosclerosis (AKA graft vascular disease) is the most important limit to the long-term success of heart transplantation. For unknown reasons, the coronary arteries of transplanted hearts undergo intimal thickening associated with hyperplasia of myocytes and fibroblasts and deposition of matrix. This results in luminal stenosis and myocardial ischemia. Patients may develop myocardial infarction, which is clinically silent because the heart is denervated. The overall survival after heart transplantation is 80% at 1 year and 60% at 5 years. Do not confuse graft arteriosclerosis with graft atherosclerosis (choice C). Atherosclerosis is caused by accumulation of cholesterol esters and development of atheromas. Atherosclerosis may recur in the coronary arteries of transplanted hearts, but is not a limiting factor in long-term success of heart transplantation. Allograft rejection (choice A) is certainly a major postoperative problem. However, thanks to early diagnosis based on periodic endomyocardial biopsy and the availability of immunosuppressant therapy, this complication can be prevented or successfully treated. Although opportunistic infections (choice D) and development of Epstein-Barr related lymphomas (choice E) are undesired effects of profound immunosuppression, these complications do not constitute a significant limitation to the overall outcome of cardiac transplantation.
30The correct answer is C. Medulloblastoma is the only tumor on the list characterized by both neuronal and glial differentiation. This tumor tends to form gray-white masses in the cerebellum of children and in the cerebral hemispheres of adults. Histologically, the tumor forms sheets of densely packed, poorly differentiated small cells. Occasional cells show spindle cell morphology and stain for the glial marker glial fibrillary acidic protein (GFAP). Other occasional cells show neuronal differentiation and form rosettes. The tumor has a 50% 10-year survival rate when treated with combined surgery and radiation. Astrocytoma (choice A), glioblastoma multiforme (choice B), and oligodendroglioma (choice C) are pure glial tumors. Meningioma (choice D) is a tumor of the meninges.
31The correct answer is E. The normal blood hemoglobin concentration is about 15-16 g/dL for a man and about 13-14 g/dL for a woman. A patient is considered to be severely anemic when the hemoglobin concentration falls below 7.5 g/dL. In severely anemic patients, the resting cardiac output is significantly increased with an increase in both heart rate and stroke volume (choice C). The increase in stroke volume causes a widening of the pulse pressure, because when a greater amount of blood is ejected during each systole, the blood pressure rises and falls to a greater extent. Bradycardia (choice A) is said to occur when the heart rate falls below 60 BPM. Severely anemic patients exhibit tachycardia, which is defined as a heart rate greater than 100 BPM. Cyanosis (choice B) refers to a bluish color of the skin and mucous membranes that results from the presence of deoxygenated hemoglobin in the blood vessels, especially the capillaries. Cyanosis does not occur in severely anemic patients despite widespread hypoxia in the tissues because 5 grams of deoxygenated hemoglobin must be present in each 100 mL of blood to produce overt cyanosis. In other words, the hemoglobin concentration is too low for a severely anemic patient to become cyanotic. The hands of anemic patients are often cold (choice D) because of decreased blood flow to the skin.
32The correct answer is C. Patients receiving heart transplants are prone to develop a number of complications, the most serious of which is graft vascular disease, AKA graft arteriosclerosis. This complication develops years after transplantation and is due to intimal thickening of coronary arteries without associated atheroma formation or significant inflammation. Thickening of the arterial intima is due to proliferation of fibroblasts and myocytes and leads to progressive stenosis of the lumen. Since transplanted hearts are denervated, chest pain does not accompany the ischemic injury. Graft vascular disease is of unknown etiology and cannot be prevented with current immunosuppressant therapy. Allograft rejection (choice A) is certainly a major postoperative problem. However, thanks to early diagnosis based on periodic endomyocardial biopsy and the availability of immunosuppressant therapy, this complication can be prevented or successfully treated. Atherosclerosis of coronary arteries (choice B) is by far the most frequent cause of ischemic heart disease. Although recurrence of atherosclerosis may be observed in the transplanted heart of patients predisposed to this condition, it rarely results in sudden death 5 years after transplantation. Hyaline arteriolosclerosis (choice D) and hyperplastic arteriolosclerosis (choice E) are pathologic changes that result from chronic damage to arteriolar walls due to hypertension. Hyaline arteriolosclerosis is associated with benign hypertension and consists of thickening of the media caused by deposition of altered proteins. This change is actually not at all benign, since it leads to chronic ischemic injury to important organs, such as brain and kidneys, resulting in tissue damage (eg, nephrosclerosis in the kidney and white matter damage in the brain). Hyperplastic arteriolosclerosis follows untreated malignant hypertension. It leads to thickening of arteriolar wall media from hyperplasia of myocytes arranged in concentric layers (onion-skinning). Hyperplastic arteriolosclerosis leads to more severe and more rapid ischemic damage to kidneys, heart, and brain. Neither type of arteriolosclerosis is observed in transplanted hearts.
33The correct answer is E. The olfactory nerves can be damaged by head injury, severe infection, and tumors such as meningiomas that may compress the olfactory bulbs. Unilateral damage is often not noticed by the patient, but bilateral damage (which surprisingly can also be missed if it develops slowly) may lead to occasional bizarre errors such as that described in the question stem. The olfactory nerves are technically the neurons on the mucosal side of the cribriform plate that send processes through the plate to synapse in the olfactory bulb, which in turn sends axons to the pyriform cortex (the primary olfactory cortex). The insula (choice A) is thought to contain the primary gustatory (taste) cortex. The nucleus ambiguus (choice B) provides the special visceral efferent fibers carried by the glossopharyngeal and vagus nerves. The postcentral gyrus (choice C) contains the primary sensory cortex. The precentral gyrus (choice D) contains the primary motor cortex.
34The correct answer is B. The disease is mumps, caused by a paramyxovirus. In children, mumps causes a transient inflammation of the parotid glands, and less commonly, the testes, pancreas, or central nervous system. Mumps tends to be a more severe disease in adults than in children. Mumps in adults involves the testes (causing orchitis) and pancreas with some frequency. Pancreatic involvement can cause elevation of serum amylase. ALT (choice A) and AST (choice C) are markers for hepatocellular damage. Ceruloplasmin (choice D) is a copper-carrying protein that is decreased in Wilson's disease. CPK-MB (choice E) is the isoenzyme of CPK that is relatively specific for the myocardium. This enzyme is increased in the early stages of a myocardial infarction
35The correct answer is D. The elevated serum cardiac enzymes indicate that a myocardial infarction has occurred. The setting (patient brought in from community with typical myocardial pain) and limitation of ST elevation to a few leads are typical of transmural infarction due to occlusion of a coronary artery. In contrast, hospitalized, severely hypotensive patients typically undergo the more generalized subendocardial infarction. Prinzmetal's angina (choice A) would not cause a marked rise in serum enzymes. Stable angina (choice B) would not cause a marked rise in serum enzymes. Subendocardial infarction (choice C) usually occurs in the setting of shock and affects most EKG leads. Unstable angina (choice E) may be accompanied by enzyme elevations up to 2 times the upper limit of normal.
36The correct answer is C. Hydroxylation of proline in fibroblasts generates the modified amino acid hydroxyproline. This is an example of post-translational modification. Hydroxyproline is involved in stabilizing the three-dimensional triple helix structure of collagen. Cysteine (choice A) is unique in its ability to form a covalent disulfide bond with another cysteine residue elsewhere in the protein molecule, thereby forming a cystine residue. Such strong disulfide bonds stabilize the three-dimensional structure of the protein. Glycine (choice B) is abundant in fibroblasts since it constitutes every third amino acid in the primary sequence of collagen. However, glycine is not hydroxylated. Serine (choice D), tyrosine (choice E), and threonine can all be phosphorylated post-translationally to form phosphoserine, phosphotyrosine, and phosphothreonine, respectively. These phosphorylated amino acids are believed to play a role in signal transduction.
37The correct answer is B. Abnormal mitotic spindles can produce tripolar mitoses. These are clearly abnormal mitoses that, when present, are considered definitive evidence that a tumor is malignant rather than benign. They are therefore often searched for by pathologists evaluating a tumor. Chiasma (choice A) is the cross-like structure produced when a homologous pair of chromosomes aligns to exchange genetic material. Mosaicism (choice C) refers to a difference in genetic material in different somatic cells of the same organism. A polar body (choice D) is a daughter cell of a developing oocyte that contains almost no cytoplasm. Synapsis (choice E) is a formal name for the pairing of homologous chromosomes with which meiosis begins.
38The correct answer is E. Flow across the aortic valve is very slow and turbulent in aortic stenosis. Consequently, aortic pressure rises slowly, and peripheral pulses are of low amplitude. The flow murmur across the aortic valve is heard during systole. Diastolic murmurs (choice A) are a consequence of turbulence during ventricular filling, such as in mitral stenosis or aortic incompetence. Classically, aortic stenosis is associated with a midsystolic murmur. Heaves are due to ventricular hypertrophy, and a left parasternal heave (choice B) indicates right ventricular hypertrophy. Aortic stenosis produces left ventricular hypertrophy, and thus a sustained apical heave is felt. The S2 heart sound (choice C) is produced when the aortic valve snaps shut. S2 is soft in aortic stenosis because of the decreased arterial pressures and the intrinsically poor mobility of the aortic valve. The S3 heart sound (choice D) is associated with rapid ventricular filling, and may occur either in mitral incompetence or congestive heart failure. No extra heart sound is heard in aortic stenosis.
39The correct answer is C. This case depicts the classic picture of cardiogenic shock. This typically occurs after ischemic myocardial injury, acute valve dysfunction associated with endocarditis, blunt chest trauma, acute myocarditis, or end-stage cardiomyopathy. Left ventricular function is compromised, therefore cardiac output is diminished. Preload is increased because blood from the right side of the heart and pulmonary circulation is pumped into an already filled left ventricle (this explains the S3 and S4 sounds that presented as a midsystolic gallop). Pulmonary artery wedge pressure, measured with a Swan-Ganz catheter, reveals left atrial pressure as well as left ventricular end-diastolic pressure and is elevated in heart failure. Left ventricular failure causes increased left atrial pressure, which results in increased hydrostatic pressure in pulmonary vasculature. Once hydrostatic pressure is higher than oncotic pressure, fluid from the circulation leaks into the alveolar spaces, causing pulmonary edema and dyspnea. Eventually, the right ventricle can no longer pump blood against the increased pulmonary pressure and fails. This causes a backup of blood, which results in increased central venous pressure. Systemic vascular resistance is increased in an attempt to compensate for the diminished cardiac output. Mixed venous oxygen levels are reduced because of increased tissue demand for oxygen
40The correct answer is D. Blood flow through the coronary circulation is regulated almost entirely by the metabolic requirements of the cardiac muscle. When the oxygen consumption of the heart increases, a larger than normal proportion of the adenosine triphosphate (ATP) in the heart muscle cells degrades to adenosine. The adenosine then dilates the coronary blood vessels, increasing oxygen delivery to an adequate level. In this way, the coronary blood flow increases in direct proportion to the oxygen consumption of the heart. In aortic stenosis, the left ventricular pressure (choice B) becomes excessively high because the resistance of the aortic valve orifice is higher than normal. This increase in left ventricular pressure increases the work load on the left ventricle (choice C) because the heart now pumps blood with an elevated left ventricular pressure. The increased work load on the heart requires a greater consumption of oxygen (choice A). Under these conditions of increased cardiac work and increased oxygen consumption, one expects the cardiac tissue oxygen concentration (choice E) to be lower than normal.
41The correct answer is A. This patient has symptoms of increased intracranial pressure, ie, nausea, vomiting, and headache. This pressure is due to the location of the mass in the 3rd ventricle, which is blocking the flow of cerebrospinal fluid from the lateral ventricles into the 3rd ventricle through the foramen of Monro. All cysts and tumors listed here may be found in the 3rd ventricle, but the histologic features are consistent with a colloid cyst. Colloid cysts are thought to derive from embryologically misplaced endodermal epithelium, which explains the presence of mucin-producing ciliated cells similar to respiratory epithelium. The cyst contains mucinous fluid. It usually presents with these type of symptoms in adults, especially middle-aged patients. Craniopharyngioma (choice B) is a neoplasm arising in the suprasellar region of children and young adults. It derives from misplaced odontogenic epithelium; indeed, the tumor is histologically identical to the most common tumor of teeth, adamantinoma. Craniopharyngiomas contain abundant calcium deposits. Although histologically benign, these tumors frequently recur since complete surgical excision is rarely feasible. A cysticercus is a cyst that develops following ingestion of Tenia solium eggs in undercooked pork. The brain is one of the preferred sites of cysticercosis (choice C), and cysticerci may develop within the brain (intraparenchymal), within the ventricles, or in the subarachnoid space. The lining of a cysticercus, however, is entirely different from a colloid cyst: it consists of three cell layers, the most superficial of which resembles dome-shaped urothelial cells. An Echinococcus cyst (choice D) is caused by infestation from another cestode parasite, Echinococcus granulosus, which is acquired from dog feces. The defining feature of an Echinococcus cyst is a tiny, hooklike projection called a scolex. Scolices detach from the wall, accumulating within the cyst and producing a sandlike sediment. Liver and lungs are the usual locations of echinococcosis. Pilocytic astrocytoma (choice E) is a tumor of astrocytic origin that affects children and young adults. It usually develops either in the cerebellar hemispheres or in the hypothalamic region. In the latter location, it may grow within the 3rd ventricle. Pilocytic astrocytomas often have a cystic structure. Histologically, the tumor consists of elongated astrocytes within an abundant fibrillary background and numerous Rosenthal fibers. The wall of the cystic component is composed of glial (astrocytic) cells, usually of a reactive nature.
42The correct answer is D. This patient has sustained a hemorrhage that has destroyed her ventral pons. Descending corticospinal and corticobulbar fibers are interrupted. The patient is unable to move the facial, pharyngeal, or limb musculature, leaving her paralyzed and unable to speak. This constellation of signs and symptoms is termed "locked-in" syndrome or state because the patient is aware of being locked within her body. Only vertical eye movements and elevation of the eyelids are possible, so the patients communicate by blinking or moving their eyes. Thus, this is a pseudocoma because the reticular activating system is intact, and the patient has periods of wakefulness. During these periods she can hear and is aware of the surroundings and her neurological status. Bilateral lesions that damage substantial portions of reticular formation in the upper pons and midbrain can cause a true coma. A lesion at the level of the cervical spinal cord (choice A) would not affect speech, ocular, facial, or pharyngeal movements. Lesions of the medulla (choice B) typically involve the medial or lateral aspect. Involvement of the lateral medulla is known as the posterior inferior cerebellar artery (PICA) syndrome, or Wallenberg syndrome. Features of this disorder include dysphonia, dysarthria, and loss of pain and temperature over the ipsilateral face and contralateral body. Additional features include nystagmus and gait problems. In medial medullary syndrome, the patient has ipsilateral hypoglossal nerve paralysis, contralateral hemiparesis or hemiplegia, and possibly contralateral loss of tactile and vibration sensation from the trunk and extremities. Lesions of the midbrain (choice C) may be (1) medial, resulting in ipsilateral oculomotor nerve paralysis and contralateral hemiplegia; (2) lateral, leading to ipsilateral oculomotor nerve paralysis, contralateral cerebellar dystaxia with intention tremor, and contralateral loss of tactile sensation from the trunk and extremities; or (3) tectal, resulting in failure of upward gaze. The thalamus (choice E) is the great sensory relay station. Lesions of the thalamus can result in loss of sensations in the contralateral side of the entire body, including the face.
43The correct answer is E. This is a classic history and presentation of a subdural hematoma, which usually occurs several days to weeks following a traumatic head injury. Often the patient will have had a hospital admission with a negative workup, including x-rays and CT scans of the head. Either gradually or abruptly, the patient can experience decreasing mental status, sleepiness, focal neurologic deficits, seizures, etc. The bleeding originates from the bridging veins of the meninges and blood collects beneath the dural layer. A CT or MRI of the brain will show a semicircular, crescent-shaped opacity (blood) just below the cranium impinging on the brain tissue. Alzheimer's disease (choice A) usually develops more gradually, typically over several years (although some cases can develop over a few months). Brain metastases (choice B) could very well present like this, however, the patient will often have constitutional symptoms of cancer such as fatigue and weight loss. In a patient with a recent traumatic event, however, subdural hematoma is more likely. An epidural hematoma (choice C) differs from a subdural hematoma in that it occurs much more rapidly, usually over several hours or less. The bleed originates from the middle meningeal artery, which runs right next to the anterolateral cranium and often gets injured with a skull fracture in this location. A CT or MRI will show a circular opacity within the cranium compressing the brain tissue. Normal pressure hydrocephalus (choice D) occurs in the elderly and is associated with urinary incontinence, new onset of confusion, and gait disturbances.
44The correct answer is F. The area enclosed by the volume-pressure diagram of the left ventricle is equal to the stroke work output of the heart during its cardiac cycle. The stroke work output is therefore lower for the heart depicted by diagram A compared to the heart with valvular damage depicted by diagram B; this fact eliminates choices A-C. Diagram B shows a volume-pressure diagram from a heart in which the aortic valve is stenosed. In aortic stenosis, blood is ejected from the left ventricle through a smaller-than-normal opening. Because the resistance to ejection of blood is high, the left ventricular pressure can sometimes increase to over 300 mm Hg with normal systolic pressure in the aorta. Note in this patient that the left ventricular peak systolic pressure has increased to about 190 mm Hg. The stroke volume is equal to the difference between the amount of blood in the ventricle prior to systole (end diastolic volume) and the amount of blood in the ventricle at the end of systole (end systolic volume). Note on Diagram A that the end diastolic volume is 125 mL and the end systolic volume is 50 mL; the stroke volume is thus 75 mL. Diagram B shows that the end diastolic volume and end systolic volume have both increased by similar amounts so that the stroke volume is still equal to 75 mL after aortic stenosis; this fact eliminates choices D and E.
45The correct answer is B. This patient has all of the characteristic clinical features of dementia (memory loss, apraxia, and confusion). The intraneuronal inclusions found at autopsy are neurofibrillary tangles. These appear as intracytoplasmic aggregates with a typical flame shape and are composed of bundles of PHFs twisted around each other. PHFs result from abnormal phosphorylation of a microtubule-associated protein called tau. Normally, tau is a soluble protein that regulates tubulin polymerization. Excessive or abnormal phosphorylation converts tau into an insoluble protein that precipitates as PHFs, filling the cytoplasm of neurons and disrupting axoplasmic transport. APP is a normal transmembrane protein of obscure function; the gene for APP is on chromosome 21. Ab amyloid is a 40 amino acid residue protein that originates from APP and forms the core of senile plaques. Abnormal degradation of APP (choice A) is thought to be the crucial event leading to formation of Ab amyloid in sporadic and familial Alzheimer disease, while increased expression of APP (choice D) leads to accumulation of Ab amyloid in the brains of patients with trisomy 21. Neither mechanism is the direct cause of PHF formation. Advanced glycosylation end (AGE) products (choice C) are insoluble proteins (mostly collagen and other long-lived proteins) that accumulate progressively in vessel walls as a result of glycosylation. This is a mechanism underlying damage in diabetes mellitus and aging, but not in PHF formation. The function of tubulin, which is the main component of microtubules, is probably altered in Alzheimer disease as a result of abnormal phosphorylation of tau and formation of PHFs. However, precipitation of insoluble a-tubulin (choice E) has not been shown to occur in Alzheimer disease.
46The correct answer is C. Citrate is produced by citrate synthase from acetyl CoA and oxaloacetate. This reaction takes place in the mitochondria, but citrate can move freely from the mitochondria into the cytosol. When the citric acid cycle slows down, citrate accumulates. In the cytosol, it acts as a negative allosteric regulator of phosphofructokinase I, the enzyme that catalyzes the committed step of glycolysis. Fructose-2,6-bisphosphatase (choice A) breaks down fructose-2,6-bisphosphate, a potent allosteric activator of phosphofructokinase I. Fructose-2,6-bisphosphatase is activated by cyclic AMP-dependent protein kinase. Isocitrate dehydrogenase (choice B) converts isocitrate to alpha-ketoglutarate in the citric acid cycle. It is allosterically stimulated by ADP and inhibited by ATP and NADH. This reaction produces NADH and CO2. Pyruvate carboxylase (choice D) is a mitochondrial enzyme that converts pyruvate to oxaloacetate. It is important in gluconeogenesis and replenishes the oxaloacetate in the citric acid cycle. 6-phosphogluconate dehydrogenase (choice E) converts 6-phosphogluconate to ribulose 5-phosphate in the pentose phosphate shunt pathway.
47The correct answer is A. The vagus nerve, through its auricular branch, supplies the posterior half of the external auditory hiatus. Since the vagus also supplies many chest and abdominal organs, reflex symptoms may occur, including fainting (typically in the elderly), cough, and gagging. The auriculotemporal nerve (choice B) supplies the anterior half of the external auditory meatus and the facial surface of the upper part of the auricle. The greater auricular nerve (choice C) supplies both surfaces of the lower part of the auricle. The lesser occipital nerve (choice D) supplies the cranial surface of the upper part of the auricle. The vestibulocochlear nerve (choice E) supplies hearing and motion sense
48The correct answer is D. This question requires you to appreciate the key structural difference between gram-positive and gram-negative microorganisms. Most gram-negatives (other than exceptional microorganisms, such as Mycoplasma, that lack a cell wall) have a more complex cell envelope than gram-positive microorganisms. It includes both a cytoplasmic membrane as well as an outer membrane. Between these two membranes is the periplasmic space, which contains enzymes such as phosphatase and penicillinase, binding proteins for the transport of various nutrients, and peptidoglycan, as well as a portion of the lipoprotein that firmly anchors the outer membrane to the peptidoglycan. Gram-positives do not have outer membranes. Choice A, the cell envelope, is incorrect because both gram-positive and gram-negative microorganisms have this structure, which is defined as all the layers that enclose the cytosol of the bacterium. It is the composition of the envelope that differs between gram-positives and gram-negatives. Choice B, exotoxin, is not exclusive to gram-negative microorganisms, but is also found in some gram-positives. By contrast, endotoxin (lipopolysaccharide; LPS) is found exclusively in gram-negatives. Choice C, peptidoglycan, is found in the cell walls of both gram-positive and gram-negative microorganisms. Note that there is a larger amount of peptidoglycan in gram-positive microorganisms. Choice E, teichoic acids, are found exclusively in gram-positive organisms.
49The correct answer is C. The circle of Willis is a series of arterial anastomoses that circle around the pituitary stalk at the ventral surface of the brain. If any of the vessels of the circle of Willis become blocked, blood can be routed through the remaining vessels. The object of this question is to determine which vessel does not belong to the circle of Willis. Of the options listed, only the middle cerebral artery does not belong to the circle, and instead courses laterally to supply the entire lateral convexity of the brain. Therefore, ligation of this vessel would produce the most ischemic damage.
50The correct answer is E. What links rheumatoid arthritis (RA) to restrictive cardiomyopathy? Amyloid! Long-standing inflammatory conditions such as RA are associated with deposition of a form of amyloid known as AA (amyloid-associated protein), which may involve kidneys, heart, liver, skeletal muscle, and skin, for example. Amyloid deposition in the myocardium results in decreased compliance and impaired diastolic filling, i.e., restrictive cardiomyopathy. The myocardium has a rigid and waxy texture. This form of amyloid, as well as any other biochemical form, can be visualized on tissue section by staining with Congo red, which acquires a characteristic apple-green birefringence under polarized light. Constrictive pericarditis (choice A) is due to any pathologic process that results in fibrous thickening of the pericardium, with resultant impaired compliance. Clinically, therefore, this condition manifests with a picture similar to restrictive cardiomyopathy because of impaired diastolic filling. Constrictive pericarditis is usually caused by previous episodes of acute pericarditis, especially hemorrhagic, suppurative, and caseous pericarditis. Dilated cardiomyopathy (choice B) is characterized by massive ventricular dilatation and may be caused by genetic alterations, myocarditis, toxic insults (alcohol), metabolic disorders (hemochromatosis), etc. Most cases are idiopathic. The main pathophysiologic alteration is impaired contractility. You may be tempted to think that this patient is prone to developing hypersensitivity myocarditis (choice C), but this form of myocardial disease has been reported after treatment with some antihypertensive agents, antibiotics, and diuretics -- not with corticosteroids or NSAIDs. Furthermore, myocarditis manifests acutely with arrhythmias and heart failure, and chronically with dilated